Abstract
Background
For patients receiving high dose cytarabine (HiDAC) at the University of Virginia Health System between 10/2019 and 10/2020, median length of stay (LOS) from time of clinic appointment to hospital discharge exceeded the expected standard treatment time (119.4 hours vs 112 hours). Despite the final dose of chemotherapy being scheduled for completion by 9:00 am on the planned day of discharge, only 50% of patients receiving HiDAC were successfully discharged by 12:00 pm (3 hours post-chemotherapy completion). Though there are no national standards for duration of inpatient stay for planned chemotherapy, LOS that extends beyond the standard treatment time results in increased cost, overutilization of hospital resources, delayed admissions for future patients, and patient dissatisfaction.
Methods
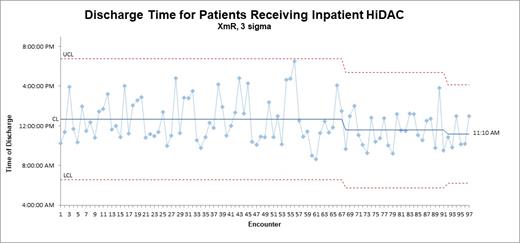
A multidisciplinary team of licensed providers, pharmacists, and nurses was formed. Due to inconsistency in admission times, the team focused on the percentage of patients discharged by 12:00 pm as a surrogate marker for LOS. The aim was to increase the percentage of patients discharged by 12:00 pm to 65%. Reviewing the baseline data revealed an unstable process with a 3-sigma XmR statistical process control chart. The team developed current and ideal process state maps, a Pareto chart, and a priority matrix to determine an action plan. The most common identified causes for delay in discharge included: lack of standardized discharge checklist, discharge order placed after 10:00 am, medications dispensed from the outpatient pharmacy after 11:00 am, licensed providers not prioritizing patients who were pending discharge, and medication reconciliation not completed prior to day of discharge.
Results
From 10/2020 to 5/2021, the first PDSA cycle focused on standardizing the discharge process to correct the instability in the process. A discharge checklist was created based on the ideal process map, which allowed providers to have a consistent process at discharge. A 3-sigma XmR chart demonstrated a newly stable process and an increase in percentage of patients discharged by 12:00 pm to 58% (14 of 24). The second PDSA cycle from 6/2021 to 8/2021 addressed the high impact/easy effort interventions identified in the priority matrix: providers completed medication reconciliation the day before discharge, prioritized seeing HiDAC discharge patients first during morning rounds, and ensured discharge orders were placed prior to completion of the last chemotherapy infusion. Following these interventions, the percentage of patients discharged by 12:00 pm increased to 66% (4 of 6).
Conclusions
Using quality improvement methodology, a multidisciplinary team developed an action plan for patients receiving HiDAC that has increased the percentage of patients discharged by 12:00 pm. This outcome may lead to decreased length of stay, reduced hospitalization costs, and increased bed availability for other hematology/oncology patients. Further PDSA cycles are planned and will focus on the pharmacy medication delivery service, and continuous evaluation of the process is ongoing.
El Chaer: Amgen: Honoraria, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal